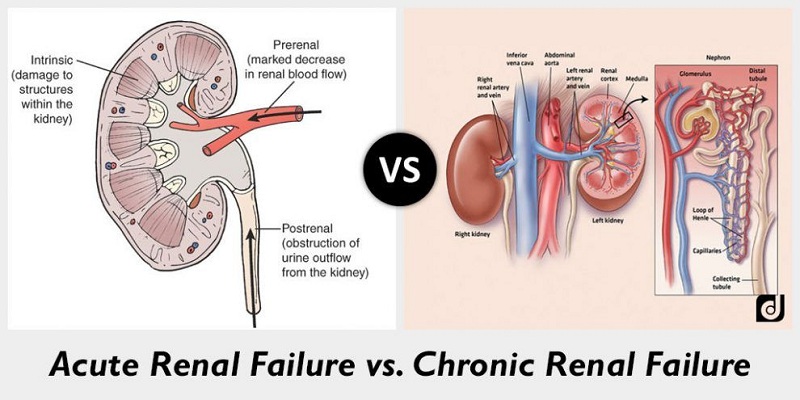
Chronic renal failure (IRC) is the gradual and progressive loss of renal function. It is due to different kidney diseases such as glomerulonephritis, pyelonephritis, bladder-ureteral reflux, calculosis and other infectious diseases, hereditary diseases such as polycystic kidney, or be secondary to other diseases such as diabetes and some autoimmune diseases, severe hypertension, diseases that cause an obstacle to normal urinary outflow, use of nephrotoxic drugs like many pain-relieving drugs. These diseases gradually produce loss of renal tissue, resulting in a metabolic clinical condition called uremia, up to the total absence of kidney function. There is no specific therapy to counter the loss of renal function, but there are different means by which we can slow down its progression and allow a better quality of life. When the renal function has reached minimum levels the patient will have to undergo a dialysis treatment in order to continue living.
Precisely because this process is slow, our body becomes accustomed to this metabolic clinical situation, and many patients come to need dialysis without knowing they have kidney disease.
Table of Contents
ToggleHere We Share Some Information for the Patient with Chronic Renal Failure:
The kidneys perform different actions:
- Removal of waste products and toxic products (slag produced by the consumption of energy in our organs for their work, such as nitrogen, creatinine, acid radicals, metabolites of drugs, etc.).
- Removal of excess liquids and salts.
- 3 Adjustment of blood pressure.
- Production of erythropoietin, a hormone that stimulates the production of red blood cells by the bone marrow.
- Regulation of calcium and phosphorus balance (fundamental elements for bone formation), through the production of vitamin D.
- Maintenance of a stable pH, (ie a constant and correct acidity) in the blood.
In short, the kidney ensures the harmony of the functions of our body rebalancing any situation of excess.
Chronic renal failure is, therefore, a complex pathology that causes other diseases (called secondary, therefore), such as hypertension, anemia, a multiform bone disease called generically osteodystrophy, peripheral neuropathies, gastropathy, and reduces the immunological defense that is the ability of an organism to defend itself against infectious agents.
What are the symptoms of chronic renal failure?
They are often so vague that they do not give particular worries. You may feel more tired, with less appetite, can increase the sense of thirst, the skin is dehydrated, the hair may become more fragile, bone pain can arise, there may be insomnia. Almost constantly arterial hypertension is present, sometimes difficult to control, diuresis becomes more abundant and it is necessary to get up even at night to urinate; only in the most severe phase of renal failure and acute renal failure can a contraction of diuresis appear.
How to diagnose the chronic renal failure?
Few tests are essential: urine tests with proteinuria, azotemia, and creatininemia make it possible to make an initial diagnosis. Your doctor may investigate further with other tests (such as a blood count to assess whether anemia has already appeared, your blood sugar to see that you have not become insulin resistant or electrolytes such as sodium, potassium, calcium, and phosphorus to see that there are alterations of these substances). It is essential to rely on a nephrologists’ who will research the cause of your illness with a renal and bladder ultrasound and with further instrumental and hematochemical examinations and will follow the evolution over the years with the most appropriate investigations prescribing the appropriate treatment of the complications of the insufficiency chronic renal.
What Can We Do?
- Check your blood pressure properly
- If you are diabetic, always keep your blood sugar level, your diet and your insulin normal.
- Avoid nephrotoxic drugs
- Cure high cholesterol and triglycerides with diet and then with appropriate therapy
- Do not smoke
- Prevent infections.
- Moderately hypoproteic diet to lighten the work of the kidney and regulate the intake of salts such as sodium, potassium, phosphorus.
Let’s see the various points one by one
Check the blood pressure properly:
Arterial hypertension is one of the most important factors that negatively influence the progression of kidney damage in patients with chronic renal failure. The high pressure, in fact, damages the arteries of all the organs but in particular of heart, kidney, eye, and brain predisposing to the risk of cardiac pathologies, stroke or cerebral hemorrhages, damages to the retina beyond the renal insufficiency. It often manifests itself with headaches and dizziness but sometimes it does not give any symptoms.
To reduce hypertension and maintain optimal pressure values (120/80 mmHg), different types of drugs are used. Your doctor will recommend the drugs that best suit your situation. These drugs must be taken on a regular basis even when the blood pressure has normalized since the pressure is kept normal thanks to the drugs. There are different classes of antihypertensives and each class has different types of drugs. Diuretics (furosemide, torasemide), stimulate diuresis, then urinate more avoiding edema and hyperhydration, calcium antagonists reduce the resistance of small arteries, giving a vasodilatation,
All of these drugs have their contraindications and their side effects, and each of us responds differently to the use of each drug. What has worked wonders with the neighbor could cause you serious trouble, always ask your doctor before taking a drug.
We have said that the optimal values of arterial pressure are 120 of maximum (systolic) and 80 of minimum (diastolic), but are accepted as normal values up to 130/85; in addition, values between 135-140 systolic and 85-89 diastolic and hypertension values over 140/90 are considered at the limits.
Salt reduction and weight loss if you are overweight will help you to control blood pressure if the values are not very high and to control it better using fewer drugs if the pressure is high. So you prefer fresh foods to canned foods (salt is used as a preservative), fresh or seasoned cheeses or cheese and cheese; do not add salt to cooked foods and salads, used to flavor the aromatic herbs and a little lemon or vinegar, drink non-carbonated water (throw away the bags of hydrolysate), in short, start getting used to a style of food a little different compared to the previous. Know that it is better to reduce the normal salt (sodium chloride) than to buy that of the pharmacy (potassium chloride) which is contraindicated in patients with renal insufficiency.
Diabetes is one of those diseases that most easily lead to kidney failure.
The first sign of kidney impairment is the appearance of minimal doses of albumin in the urine, the search for microalbuminuria in these patients is a specific test to be taken in addition to urine examination and normal proteinuria.
The diabetic patient must constantly maintain a normal blood sugar level, with the help of diet therapy and hypoglycemic drugs to prevent the onset of renal failure.
When renal failure is present the drug to be used is only insulin.
If there is no diabetes but only an insulin resistance is recommended to first of all strictly comply with the diet, eliminating simple carbohydrates, ie sugar, honey, sweets and use sparingly complex carbohydrates such as bread, pasta, rice and flour in general.
Avoid nephrotoxic drugs
There are many drugs that can cause renal failure and promote faster progression, so they should be used with particular care.
The so-called NSAIDs (non-steroidal anti-inflammatory drugs) are the most used drugs for pain (nimesulide, ketoprofen, diclofenac, ibuprofen, naproxen, piroxicam, ketorolac, meloxicam, sold with fanciful commercial names). Such drugs can cause harm, reducing the blood supply to the kidney, with increased creatinine, atrophy and blood pressure. This condition can also be non-recoverable.
There are other drugs that have an anti-pain and anti-inflammatory action, but they interfere less with renal metabolism. Always ask your doctor about the most appropriate drug for your problem, and remind him that you have a kidney failure.
Among the antibiotics, aminoglycosides (amikacin, gentamicin, kanamycin, neomycin, tobramycin, streptomycin) are eliminated inactive form exclusively by the kidneys and can cause damage to the structures of the kidney (nephrotoxicity). In patients with renal insufficiency, these drugs tend to accumulate) also causing damage to the inner ear (dizziness and deafness).
For other antibiotics of more common use such as those of the cephalosporins and quinolone and fluoroquinolones in the presence of renal insufficiency, it is necessary to reduce the dose for which it is advisable to strictly follow the instructions of the doctor.
Other drugs can also be harmful to patients with renal insufficiencies, such as potassium-sparing diuretics that may cause hyperkalemia, should only be given by specialist prescription. Oral antidiabetics in advanced renal failure may give hypoglycaemic crises because they are eliminated predominantly by the kidneys.
Even if some drugs are not used in radiology for contrast studies (such as urography, tac, etc) called iodinated contrast agents, they can seriously worsen chronic renal failure or cause acute renal failure in patients who are dehydrated or diseases such as diabetes or myeloma. Before undergoing such examinations it is good to feel the nephrologist and plan a protective therapy.
Treating dyslipidemia
That is, changes in cholesterol and triglycerides that often accompany chronic renal failure. Dyslipidemia causes the formation of atherosclerotic plaques in the arteries, can cause coagulation abnormalities, and thrombosis. First of all, it is necessary to correct food errors by reducing the quantity of foods, moderating fats, cholesterol-rich foods, cheeses, preferring vegetables and fruit. If you are overweight you need to lose weight and get used to constantly doing a little ‘movement (walking briskly, cycling, swimming, exercises to strengthen the column etc.) In short, review the habits and create a new way to feed and live. The first cure is, therefore, the diet, to be done for at least six months, only later can you resort to drugs. The most used are statins, and then there are the clofibrate and the omega three for hypertriglyceridemia. The doctor will prescribe the most suitable one for you.
Abolish the smoke
In fact, it causes vasoconstriction in the arterioles damaging them. In patients with renal insufficiency, smoking also causes a reduction in blood supply in the kidney capillaries, causing hypoxia (oxygen reduction) that can damage the kidney. At the level of the lower limbs, it causes a well-known pathology, Burger’s disease, which can cause lesions that make amputation necessary. Equally, important damage can give lung and bladder, in fact, smoking increases the risk of lung and bladder tumors. The association between smoking and arterial hypertension enhances renal damage. It is really important therefore to stop smoking.
Preventing infections.
All infectious facts can lead to worsening of renal failure. We, therefore, recommend the maximum precaution when there are influenza epidemics, avoiding very crowded places. If cystitis or episodes of pyelonephritis due to bladder-ureteral reflux occur frequently, do not wait to go to the toilet when you have the urinary urgency but go to urinate at intervals of a few hours, and observe a thorough personal hygiene. Do not neglect any kind of infection: your family doctor will advise you on the most suitable therapy.
Diet is one of the therapies of chronic renal failure.
It is not a diet to lose weight but a diet that reduces the amount of protein allows the kidney a lower workload, allows the control of the amount of some substances that can become dangerous in renal failures, such as sodium, phosphorus, and potassium, and allows a better regulation of the pH of the blood.
With this diet, we try to give an optimal intake of calories so that the body has the energy necessary to work and make better use of the proteins introduced. All foods give us calories, fat in greater quantities. The recommended calorie intake is 30-35 Kcal per pound of ideal weight, obviously if you are not overweight or obese.
It limits the amount of protein to that necessary for the constitution of the muscles, the reconstruction of damaged tissues and the processing of vital proteins (hormones, enzymes, immunoproteins). It is, therefore, necessary that the proteins are of first quality and that is why we prefer the animal proteins, better used by our organism compared to the vegetable proteins. Proteins are found in animal products such as meat, fish, eggs and milk and dairy products, and in plant products such as grains, legumes, and dried fruit. Protein restriction is different depending on the severity of renal failure.
Consider that the daily intake in a habitual diet is around 1.2-1.5 grams and more protein per pound of weight and that the income of at least 0.75 grams for normal growth is considered essential. In the early stages a modest restriction is recommended, 1-0.8 grams, then as the renal failure becomes more severe, the protein restriction becomes more important, up to 0.6 grams and in some diets even 0.3 with of amino acid supplements.
It is therefore advisable to adjust the protein intake with the diet for several reasons:
- Relieves symptoms related to hyper azotemia (increased levels of nitrogen in the blood), such as nausea, vomiting, loss of appetite and physical tiredness.
- Slows the loss of renal function
- Reduces the accumulation of phosphorus (implicated in the pathogenesis of uremic osteodystrophy)
- Helps to prevent metabolic acidosis (reduction of the pH in the blood)
- Participates in the maintenance of a satisfactory nutritional status.
In patients with very advanced renal insufficiency, in a low protein diet, one can associate the use of protein products (without proteins), such as pasta, bread, rusks, biscuits, milk. This allows reducing the sense of hunger, introducing greater quantities of food, without increasing the load of proteins and to use food of animal origin as a protein source.
Modern studies have documented that a good nutritional condition of the patient with chronic renal failure reduces the risk of mortality and increases the quality of life. Therefore, most doctors, including us, have abandoned excessively restrictive diets, which can lead to undernutrition.
The diet also controls the intake of potassium. The kidney plays an essential role in regulating the concentration of potassium in the blood, controlling its elimination. In chronic renal failure, especially in the more advanced stage, this capacity is reduced, so potassium tends to accumulate in the blood. Since potassium controls the ability to contract muscles, including the cardiac one, the increase in potassium (hyperkalemia) can cause alterations of the cardiac rhythm (arrhythmias), of the different entity, until the cardiac arrest.
We, therefore, understand that it is very important to avoid or in any case reduce the ingestion of foods with a high content of potassium. But which foods contain potassium?
All foods, especially fruits and vegetables, contain potassium, but very rich are all dried and dried fruit, legumes both fresh and dried, potatoes, black olives, broccoli, artichoke spinach, cauliflower, sprouts, mushrooms, bananas apricots, avocado, banana, coconut, kiwi, melon.
We recommend to cook the vegetables in abundant quantities of water, to drain it well and to repeat the operation a second time; this allows to eliminate a greater quantity of potassium.
To avoid the risk of hyperkalemia a drug can be used, a resin that binds to potassium and reduces its absorption in the intestine. Hyperpotassemia is often associated with a situation of metabolic acidosis (accumulation of acids in the blood). If this alteration is found at laboratory tests, it is important to take sodium bicarbonate.
The hypoproteic diet also reduces the intake of phosphorus. Calcium and phosphorus are two minerals of fundamental importance for the human organism; maintaining their bone health depends on their balance. In the most advanced phase of chronic renal failure there is a reduced renal elimination of phosphorus but also a reduced production of vitamin D (responsible for low levels of calcium in the blood), therefore we see an imbalance between these two minerals, (ie calcium it is low and the phosphorus is high).
This condition is a stimulus for the production of parathormone (a hormone that together with vitamin D regulates the formation and structure of the bone) by the parathyroid glands (endocrine glands located in the neck). This represents the basis of hyperparathyroidism and uremic osteodystrophy, a bone pathology characterized by a weakening of the bone, which can cause bone pain, spontaneous fractures, and deformations. All of this can obviously have a negative effect on the quality of life of patients. It is therefore important, in the most advanced stages of chronic renal failure, to contain the accumulation of phosphorus, reducing its intake with the diet. The control of the phosphorus in the blood, in fact, allows maintaining appropriate levels of vitamin D so that calcium is also at adequate levels.
Where is phosphorus contained? In all foods that contain protein, but the richest foods in phosphorus are dried vegetables, cheeses, chocolate, nuts. Some meat (turkey, horse), some types of fish such as salmon, and crustaceans, in general, have a considerable phosphorus content. The egg yolk is very rich in phosphorus. It also has a high phosphorus content including some drinks like coca cola and grapefruit and orange juice. The boiling of food in two glasses of water, as for potassium, allows us to eliminate high levels of phosphorus. Recall that preserved foods (canned foods, sliced cheese or cheese, sausages) contain phosphorus as a polyphosphate as a preservative.
To reduce hyperphosphatemia (accumulation of phosphorus in the blood) we have some medicines available, such as calcium carbonate, calcium acetate, and sevelamer. At the intestinal level, these preparations bind to phosphorus, preventing their absorption.
Sodium control is also important for the patient with chronic renal failure and we have already discussed this in the chapter on hypertension.
One of the functions of the kidney is the control of the balance of liquids in the body.
In chronic renal failure, there is a progressive loss of this capacity, so liquid retention (hyperhydration) can occur. This retention is exacerbated by the excessive use of salt. All of this can cause an increase in blood pressure due to increased blood volume. If the excess liquids reach high levels (over 2-3 liters), the edemas appear (swelling), first in the most sloping areas of the body (feet and legs). If this condition is not recognized and, therefore, adequately treated, one can have a picture of pulmonary edema (accumulation of fluid in the lung), with important difficulty in breathing the patient.
To facilitate diuresis and reduce the condition of edema must first reduce the intake of salt, then there are drugs called diuretics, which stimulate the kidney to eliminate more water. The patient must drink according to the sense of thirst, checking the number of liquids introduced, both in terms of drinks and food (soups, fruits, vegetables, ice cream), his diuresis (daily quantity of urine) and his body weight, measuring it in the morning.
To conclude the prevention of chronic renal failure and the slowing of its evolution must provide a different view of the way of life and food.
Useful Tips:
- Adequate control of blood pressure. Maintain optimal blood pressure values by reducing the intake of salt and alcohol and/or using antihypertensive drugs.
- Cook with a little salt and add a little salt in food, prefer fresh food to those stored
- Pay attention to animal fats preferably use olive oil.
- Drinking according to the sense of thirst, without drinking excess in an attempt to increase diuresis, control body weight in the morning before breakfast. The increase of 1 kg of body weight or more in a short time (a few days), the appearance of swelling, or the reduction of diuresis, should not be underestimated, you must resort to the specialist doctor.
- If you are diabetic, check your blood sugar carefully.
- Dairy products and cheeses, (rich in phosphorus) must be kept to a minimum. The dry cheeses (Parmigiano and pecorino) can be used in very small quantities (not over 5 gr.) To flavor pasta or rice.
- Attention to drugs. Do not take anti-inflammatories without the advice of the nephrologist.
- Do not smoke
- Perform a constant physical activity.
Warning:
This material gives you general information and does not replace the doctor’s advice. You should contact your doctor to ask him any questions related to your health, therapy or treatment.
You may also like to read this content Homemade smoked salmon: how to prepare it?